Search
- Page Path
- HOME > Search
Original Article
- Indications for open hepatectomy in the era of laparoscopic liver resection: a high volume single institutional study
- Sung Jun Jo, Jinsoo Rhu, Jong Man Kim, Gyu-Seong Choi, Jae-Won Joh
- J Liver Cancer. 2022;22(2):146-157. Published online September 14, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.22
- 2,305 Views
- 60 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Since the introduction of laparoscopy for liver resection in the 1990s, the performance of laparoscopic liver resection (LLR) has been steadily increasing. However, there is currently no data on the extent to which laparoscopy is used for liver resection. Herein, we investigated the extent to which laparoscopy is performed in liver resection and sought to determine whether surgeons prefer laparoscopy or laparotomy in the posterosuperior (PS) segment.
Methods
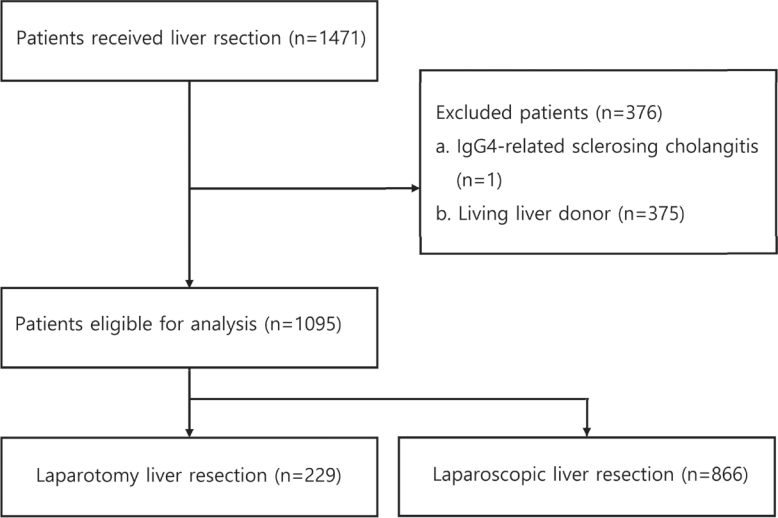
For this retrospective observational study, we enrolled patients who had undergone liver resection at the Samsung Medical Center between January 2020 and December 2021. The proportion of LLR in liver resection was calculated, and the incidence and causes of open conversion were investigated.
Results
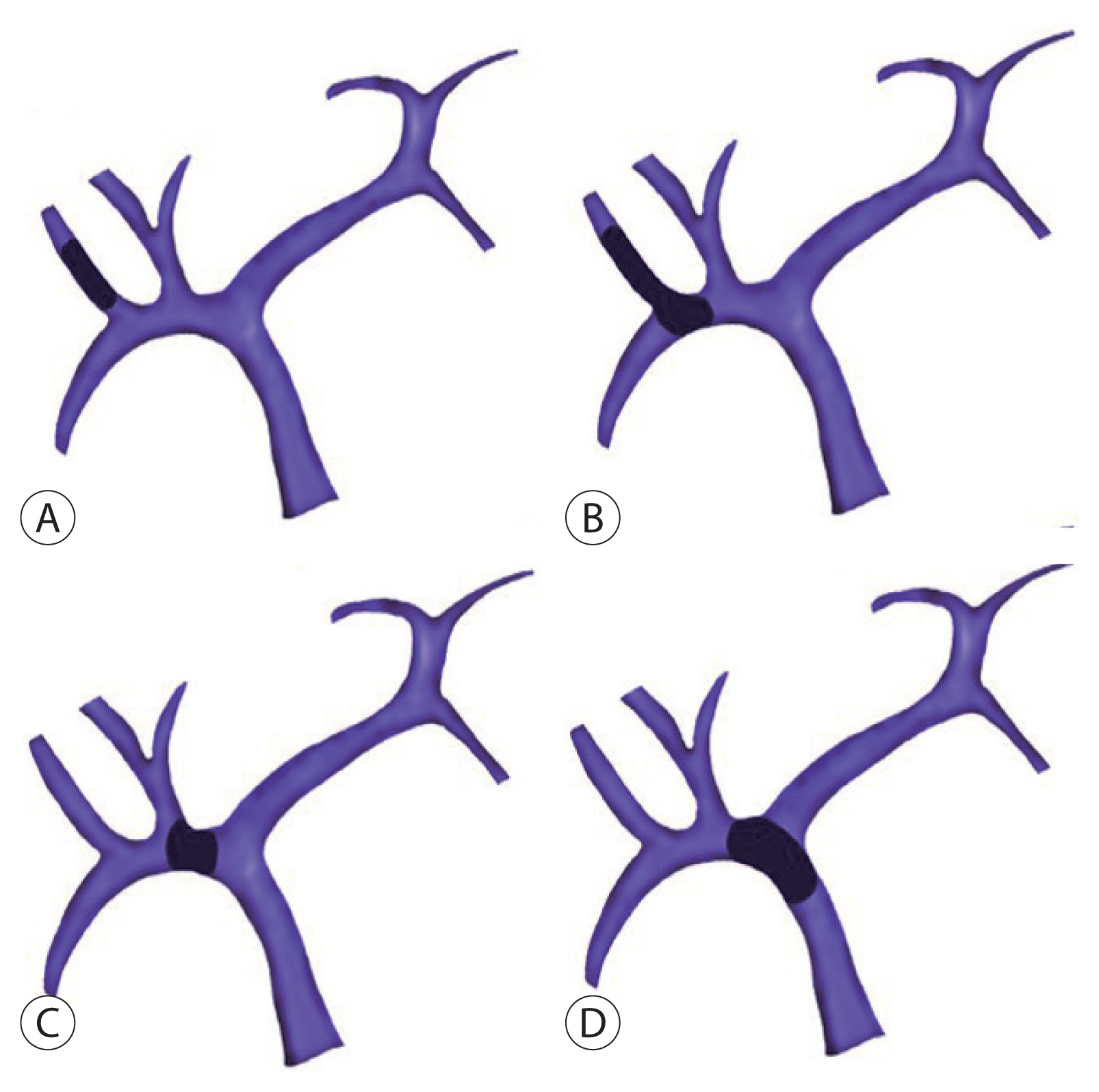
A total of 1,095 patients were included in this study. LLR accounted for 79% of the total liver resections. The percentage of previous hepatectomy (16.2% vs. 5.9%, P<0.001) and maximum tumor size (median 4.8 vs. 2.8, P<0.001) were higher in the open liver resection (OLR) group. Subgroup analysis revealed that tumor size (median 6.3 vs. 2.9, P<0.001) and surgical extent (P<0.001) in the OLR group were larger than those in the LLR group. The most common cause of open conversion (OC) was adhesion (57%), and all OC patients had tumors in the PS.
Conclusions
We investigated the recent preference of practical surgeons in liver resection, and found that surgeons preferred OLR to LLR when treating a large tumor located in the PS. -
Citations
Citations to this article as recorded by- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef - A systematic review and meta-analysis of blood transfusion rates during liver resection by country
Seonju Kim, Yun Kyung Jung, Kyeong Geun Lee, Kyeong Sik Kim, Hanjun Kim, Dongho Choi, Sumi Lee, Boyoung Park
Annals of Surgical Treatment and Research.2023; 105(6): 404. CrossRef
- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis

Review Article
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Sang Jin Kim, Jong Man Kim
- J Liver Cancer. 2021;21(2):105-112. Published online September 2, 2021
- DOI: https://doi.org/10.17998/jlc.2021.03.17
- 5,003 Views
- 221 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Traditionally, liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis is not recommended. However, with recent developments in locoregional therapies for hepatocellular carcinoma, more aggressive treatments have been attempted for advanced hepatocellular carcinoma. Recently, various studies on locoregional therapies for downstaging followed by living donor liver transplantation reported inspiring overall survival and recurrence-free survival of patients. These downstaging procedures included three-dimensional conformal radiation therapy, trans-arterial chemoembolization, stereotactic body radiation therapy, trans-arterial radioembolization, hepatic arterial infusion chemotherapy and combinations of these therapies. Selection of the optimal downstaging protocol should depend on tumor location, biology and background liver status. The risk factors affecting outcome include pre-downstaging alpha-fetoprotein values, delta alpha-fetoprotein values, disappearance of portal vein tumor thrombosis on imaging and meeting the Milan criteria or not after downstaging. For hepatocellular carcinoma with portal vein tumor thrombosis, downstaging procedure with liver transplantation in mind would be helpful. If the reaction of the downstaged tumor is good, liver transplantation may be performed.
-
Citations
Citations to this article as recorded by- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy
Hun Kim, Tae Hoon Roh, Jun Seop Lee, Min Seong Kim, Beom Kyung Kim
Journal of Liver Cancer.2024; 24(1): 113. CrossRef - Refining MRI-based criteria for portal vein invasion in hepatocellular carcinoma: improving sensitivity beyond portal vein tumor thrombosis
Jeongju Kim, Woo Kyoung Jeong, Jong Man Kim, Sang Yun Ha, Kyunga Kim
Abdominal Radiology.2023; 49(2): 437. CrossRef - Prediction models of hepatocellular carcinoma recurrence after liver transplantation: A comprehensive review
Sang Jin Kim, Jong Man Kim
Clinical and Molecular Hepatology.2022; 28(4): 739. CrossRef
- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy

Case Report
- Hepatocellular Carcinoma Arising from Hepatocellular Adenoma in an Elderly Male Patient
- Manuel Lim, Jong Man Kim, Ji Eun Kwon, Eun Sung Jeong, Jaehun Yang, Okjoo Lee, Kyeong Deok Kim, Sang Jin Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
- J Liver Cancer. 2021;21(1):87-91. Published online March 31, 2021
- DOI: https://doi.org/10.17998/jlc.21.1.87
- 4,000 Views
- 95 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
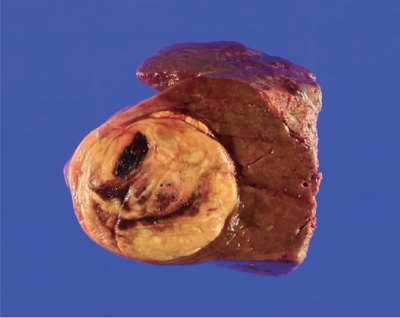
PDF - Hepatocellular adenoma is a benign tumor of the liver occurring predominantly in young women taking oral contraceptives. The malignant transformation of hepatocellular adenoma into hepatocellular carcinoma has rarely been reported. Herein, we report the case of an elderly male patient with hepatocellular carcinoma that developed from hepatocellular adenoma. The patient’s high risk for surgery and conflicting biopsy and imaging results made it difficult to determine the treatment direction. Eventually, the mass was completely removed by laparoscopic left hemi-hepatectomy without complications.
-
Citations
Citations to this article as recorded by- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef
- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis

Review Article
- Liver Transplantation in Mixed Hepatocellular Carcinoma and Cholangiocarcinoma
- Jong Man Kim
- J Liver Cancer. 2019;19(2):85-90. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.85
- 3,837 Views
- 89 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
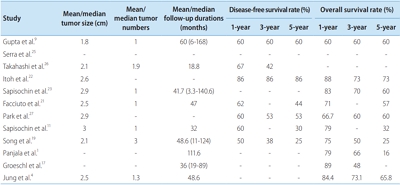
PDF - Mixed hepatocellular carcinoma and cholangiocarcinoma (HCC-CC) are rare tumors, and the risk factors associated with them are not well understood yet. Moreover, the diagnosis of mixed HCC-CC can be complicated due to the difficulty in distinguishing mixed HCC-CC from HCC and intrahepatic CCC on radiological images. Serum tumor markers are useful when the radiological images are inconclusive. It remains unclear whether the prognosis of mixed HCC-CC differs from that of HCC. However, several studies have reported that the tumor recurrence and patient survival rates of mixed HCC-CC were similar to those of HCC after liver transplantation (LT) and liver resection. In this paper, we report that LT in patients with mixed HCC-CC achieves outcomes which are similar to those seen in LT for HCC. Therefore, the diagnosis of mixed HCC-CC should not be considered as a contraindication for LT.
-
Citations
Citations to this article as recorded by- Liver transplantation for combined hepatocellular carcinoma and cholangiocarcinoma: A multicenter study
Jongman Kim, Dong-Jin Joo, Shin Hwang, Jeong-Moo Lee, Je-Ho Ryu, Yang-Won Nah, Dong-Sik Kim, Doo-Jin Kim, Young-Kyoung You, Hee-Chul Yu
World Journal of Gastrointestinal Surgery.2023; 15(7): 1340. CrossRef - The Role of Immunosuppression for Recurrent Cholangiocellular Carcinoma after Liver Transplantation
Safak Gül-Klein, Paulina Schmitz, Wenzel Schöning, Robert Öllinger, Georg Lurje, Sven Jonas, Deniz Uluk, Uwe Pelzer, Frank Tacke, Moritz Schmelzle, Johann Pratschke, Ramin Raul Ossami Saidy, Dennis Eurich
Cancers.2022; 14(12): 2890. CrossRef
- Liver transplantation for combined hepatocellular carcinoma and cholangiocarcinoma: A multicenter study


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter